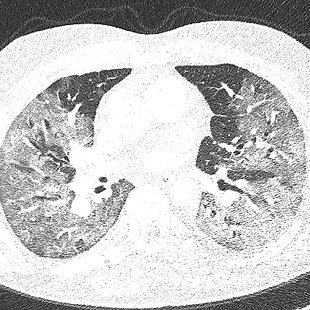
COVID-19 patient in the hospital
Coronavirus Disease 2019 (COVID-19) is currently a global problem. Patients require specific care from initial treatment in emergency departments. Many patients with extensive bilateral pneumonia require hospitalization in the intensive care unit and are dependent on high-flow oxygen therapy. In some of them, despite all treatment, lung disease progresses to the form of acute respiratory distress syndrome with the need to be connected to mechanical lung ventilation. Adequate blood gas exchange often cannot be achieved by a protective setting of mechanical ventilation. Therefore, the physician must use the prone position and, in the most severe cases, also consider the extracorporeal membrane oxygenation support. The algorithm is divided into two parts, and the participant can decide whether he wants to take care of the patient with COVID-19 during emergency admission or play the role of an intensive care physician.
Review
The disease caused by SARS-CoV-2 (COVID-19) is a highly topical issue of a pandemic nature, which leads to a great burden on the health system worldwide, and in severe forms to a significant increase in morbidity and mortality. COVID-19-based acute respiratory distress syndrome (ARDS) usually leads to a life-threatening respiratory gas exchange disorder that cannot be resolved with the protective setting of conventional artificial lung ventilation or pronation position and initiation of extracorporeal membrane oxygenation (ECMO) support should be considered. Managing the care of patients with COVID-19 on their arrival at the hospital, e.g., through the emergency room (ER) and hospitalization in the intensive care unit (ICU), is currently a key part of many health professionals’ workload not only in the Czech Republic. The presented algorithm is a clear guide on leading the management of COVID-19 patients in two levels of severity, wherein two branches logically describe health care from the ER to the ICU.
Sources
ALHAZZANI, Waleed, et al. Surviving Sepsis Campaign Guidelines on the management of adults with coronavirus disease 2019 (COVID-19) in the ICU: first update. Critical care medicine, 2021, 49.3: e219-e234. [online]. [cit. 2021-04-04]. Available at: https://journals.lww.com/ccmjournal/pages/articleviewer.aspx?year=2021&issue=03000&article=00021&type=Fulltext
FLAJŠINGROVÁ J., et al. Příjem a třídění pacientů se suspektním nebo potvrzeným COVID-19. [online]. [cit. 2021-04-01]. Available at: https://csim.cz/wp-content/uploads/07_DP_SUMMK_CSARIM_CSIM_Prijem-a-triage-pacienta-s-COVID-19-na-UP_verze_070420_final.pdf
CAPUTO, Nicholas D., Reuben J. STRAYER a Richard LEVITAN. Early Self‐Proning in Awake, Non‐intubated Patients in the Emergency Department: A Single ED’s Experience During the COVID‐19 Pandemic. Academic Emergency Medicine [online]. 2020, roč. 27, č. 5, s. 375–378. ISSN 1069-6563. [online]. [cit. 2021-04-01]. Available at: https://pubmed.ncbi.nlm.nih.gov/32320506/
BALÍK, M., et al. Použití kortikosteroidů u COVID-19. [online]. [cit. 2021-04-01]. Available at: https://csim.cz/wp-content/uploads/Kortikosteroidy-u-Covid-19_5.10.2020.pdf
JUMA, Salina; TAABAZUING, Mary-Margaret; MONTERO-ODASSO, Manuel. Clinical frailty scale in an acute medicine unit: a simple tool that predicts length of stay. Canadian Geriatrics Journal, 2016, 19.2: 34. [online]. [cit. 2021-04-04]. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4922366/
ZUCMAN, Noémie, et al. Prediction of outcome of nasal high flow use during COVID-19-related acute hypoxemic respiratory failure. Intensive care medicine, 2020, 46.10: 1924-1926. [online]. [cit. 2021-04-01]. Available at: https://link.springer.com/article/10.1007%2Fs00134-020-06177-1
COOK, T. M., et al. Consensus guidelines for managing the airway in patients with COVID‐19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia, 2020, 75.6: 785-799. [online]. [cit. 2021-04-01]. Available at: https://doi.org/10.1111/anae.15054
NATIONAL HEART, LUNG, AND BLOOD INSTITUTE ARDS CLINICAL TRIALS NETWORK. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. New England Journal of Medicine, 2004, 351.4: 327-336. [online]. [cit. 2021-04-01]. Available at: https://www.nejm.org/doi/full/10.1056/NEJMoa032193
NATIONAL HEART, LUNG, AND BLOOD INSTITUTE ARDS CLINICAL TRIALS NETWORK. Ventilator protocol card. [online]. [cit. 2021-04-01]. Available at: http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf Doporučený postup „COVID-19“ ČSARIM a ČSIM - Ventilační podpora u pacientů s COVID-19. 2020. Dostupný z: https://csim.cz/wp-content/uploads/06_DP_COVID_CSARIM_UPV_verze_1_050420_final.pdf
FERRANDO, Carlos, et al. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive care medicine, 2020, 46.12: 2200-2211. [online]. [cit. 2021-04-01]. Available at: https://link.springer.com/article/10.1007/s00134-020-06192-2
GUÉRIN, Claude, et al. Prone positioning in severe acute respiratory distress syndrome. New England Journal of Medicine, 2013, 368.23: 2159-2168. [online]. [cit. 2021-04-01]. Available at: https://www.nejm.org/doi/full/10.1056/nejmoa1214103
MÁCA, Jan. ARDS v klinické praxi. Maxdorf Jessenius, 2019. Life In The Fastlane. https://litfl.com/coronavirus-disease-2019-covid-19/