Refractory Seizures in Children
Convulsive states are one of the most common conditions which lead to admission to ICU in children. There is an inexhaustible amount of potential causes of convulsions in pediatric patients, starting with very common febrile spams to extremely rare metabolic or genetic disorders. In any case, every convulsive state always calls for quick termination. This way we can prevent the further brain damage caused by uncoordinated convulsive activity. Follow-up wide differential diagnostics are performed to determine definitive diagnosis.
Review
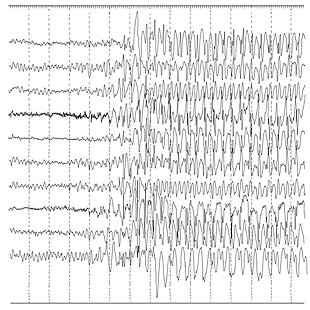
Výukový algoritmus o peroperačně vzniklé arytmii věrně kopíruje běžnou klinickou praxi, které jsme exponováni. Každý aConvulsions are defined as abnormal, stereotypical seizure-like alterations of neurological functions (motor, autonomic, behavioural). It is a common condition in the paediatric population, which can be caused by a wide spectrum of causes (neuroinfections, CNS traumas, metabolic defects, paraneoplasia, tumours, toxins, genetically related convulsive conditions). When we deal with convulsions in children, it is necessary, in addition to searching for the cause, to promptly terminate the convulsions to avoid permanent damage to the CNS. If the convulsions last longer than 5 minutes or the patient does not wake up in between two seizures, we talk about Status Epilepticus (SE). If the convulsions persist even after the use of drugs of the first (benzodiazepines) and second choice (levetiracetam, valproate, phenytoin, phenobarbital), the condition is referred to as refractory SE, which must be managed by continuous injection of anaesthetics according to the decision of the attending intensivist and neurologist (e.g. midazolam, propofol, thiopental). Convulsive activity lasting more than 24 hours is then termed super-refractory SE. The essential method in the diagnostics of convulsions is (in addition to laboratory tests and imaging methods) EEG, especially continuous EEG at the patient's bedside, which is able to detect the so-called non-convulsive state (pathological EEG recording without obvious clinical convulsions). The following algorithm clearly demonstrates the essential steps in the treatment of a child with refractory convulsions. It is an excellent educational material, which, by means of a sample case study, allows the researchers to go step by step through the necessary interventions listed above. These steps are based on the currently valid recommendations for the optimal provision of a child with refractory convulsions. nesteziolog musí znát doporučené postupy léčby arytmií a management celého operačního tímu v případě nutnosti akutní léčebné intervence, která si vyžaduje dočasné přerušení operace (jako např. v algoritmu použitá kardioverze). Je skvělé, že se díky tomuto algoritmu nad touto problematikou můžeme zamyslet a vyzkoušet si léčbu ve virtuálním prostoru.
Sources
MALÁSKA, Jan, Jan STAŠEK, Milan KRATOCHVÍL and Václav ZVONÍČEK. Intenzivní medicína v praxi. Praha: Maxdorf, [2020]. Jessenius. ISBN 978-80-7345-675-7.
GLAUSER, Tracy, et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: report of the Guideline Committee of the American Epilepsy Society. Epilepsy currents, 2016, 16.1: 48-61.
STRÝČEK, Ondřej, et al. Nová definice status epilepticus a možnosti jeho farmakologické léčby. Anesteziologie a intenzivní medicína, 2018, 29.4: 207-216.
KLUČKA, Jozef, et al. Pediatric Patient with Ischemic Stroke: Initial Approach and Early Management. Children, 2021, 8.8: 649.